|
Pelvic pain is complex and has many faces. We've talked about Painful Periods, Endometriosis and now we're going to tackle Bladder Pain Syndrome. Bladder Pain Syndrome may have begun like this: You had a urinary tract infection that just didn't go away. You felt urgency to void. You felt pain just above your pubic bones (where your bladder lives), in your perineum and/or in the urethra (the tube from the bladder to the outer world). When urinary tract infections became chronic, the old thinking was that the interstitium (bladder lining) was inflamed, ergo the outdated name "Interstitial Cystitis". Bladder Pain Syndrome is far more complex, the name far more descriptive. In 2018, we know the onset of BPS is more like this: Your bladder thinks that it's under threat…..a grizzly is at its door. Your bladder may have suffered at some point in your life, perhaps when you were a child (Chronic infections? Withholding voiding? Difficulty with bedwetting?). The part of your brain that worked with your bladder remembered this sense of distress. Later on in life (with puberty, onset of intimate relations, stressful situations, baby having, an accident or menopause), your bladder had "flashbacks" and kicked into that difficult memory. Your immune system pitched in, bringing on an immune response and inflammation. Your bladder nerve endings and the nerve pathways to the brain were woken up. Your tendons, muscles and fascia tightened up in order to protect the area. The outcome? You may develop a hypersensitive, overactive, inflamed bladder. As your bladder fills, it naturally stretches. That tight and inflamed bladder isn't so keen on stretching, sending a threat message to the brain. Your bladder naturally fills to 500-ish mls., but with BPS it can become painful at only 100 mls.. The bladder may also not welcome urine due to the inflamed lining, so you may feel a sense of urge to get rid of it…now! If you experience these feelings for more than three months, your brain begins to focus on the bladder, becoming attentive to all bladder sensations from a little urine to moderately full to urgency to pain! The natural voiding reflex and habits become distorted over time and your bladder forgets how to feel the "Oh, I'm getting full…..I'll have to go to the loo soonish, but no rush" sensation. The rising tension in the pelvic floor creates more problems. Toilet time naturally involves releasing the pelvic floor along with opening of your sphincters in a lovely dance. With a tight pelvic floor, your urine stream may become slow, interrupted, painful and incomplete. Intimacy may become painful. You may have an accompanying challenge with bowel release (not constipation….it's the letting it go part that becomes slow and/or painful). Your stress system and brain become alerted over time and this increases your perception of pain; it attaches it to your emotional state. If you haven't slept, are having a bad day or have stress, you'll feel BPS more than you would have otherwise. It's just all so connected. What can you do about it? Find a pelvic certified physio. You'll be asked about how your bladder functions, how often you void, how it feels before, during and after voiding, how your bowel works (loading, comfort, movement, frequency), pelvic floor function, deep core function and how your life is working (your nutrition, sleep, understanding of pain, pelvic systems and stress management). Your internal and external pelvis and deep core will be assessed. Research has shown us that your pelvic floor needs to be calmed down in its hypertonicity (tension), pain and function or the dysfunction and pain in your bladder won't change. You will be taught pelvic floor releases with breathing patterns, general and specific stretches and perhaps the use of a wand (a pelvic trigger point tool for you to use). An elimination diet is helpful, but no two women with BPS have the same dietary triggers. Eat food that agrees with you. Get good sleep and downtime. Find and manage your stressors. Bladder Pain Syndrome can be managed well. You can experience a cascade of wonderful changes when you take charge of your own health.
0 Comments
 "That time of the month" may bring on cramps, bloating, food cravings, unpleasant moods, loss of energy for some women. Consistently painful periods are NOT normal, so please ask for help if that is your experience and learn some ways to ease your discomfort! Deep Breathing Stress can increase period pain, make you skip or lose your periods altogether. When you're stressed or in pain, your breathe at the top of your lungs, just under your collarbones. Breathing deeply and fully into your low lungs creates rhythmic abdominal and pelvic movement. It's a natural massage, moving your organs like seaweed dances in the ocean in response to waves. Slow, relaxed deep breathing promotes relaxation, enhances your mood, improves your concentration and simply feels wonderful! Use your breath to make a simple, accessible and lovely change. Here's how: Ly on your bed with a pillow under your head and another under your knees. Let you body release and relax. Place one hand on your chest and the other on your low belly, making sure your elbows are supported on the bed. No effort! Now, breathe in slowly through your nose. Let your belly lift, your low back arch, your pubic bones descend towards your feet and your hips release. Your lower hand will have lifted and your upper hand will stay quiet on your upper chest. Now just let the air seep out of your nose, exhaling without effort. Let is be as slow as you're comfortable enjoying. Count a slow 4 counts in and at least 4 or more (to 5 or 6?) out. Repeat. Enjoy. Release Your Pelvic Floor When our body experiences pain, it may respond by tightening up and holding back. Periods, when completed with ease, are about letting go! Our pelvic floor can get in the way of releasing our flow by becoming tight in response to pain. Begin practicing release of your pelvic floor by sitting on a big ball or over an upholstered sofa/chair arm. Breathe into your low belly, feel your pelvic floor open and release…….use this technique when you're in your painful cycle and you will find more ease with your flow. Abdominal Massage Start with a hot water bottle or heated wheat bag for 15 - 20 minutes in a restful position and quiet place. Cover yourself with a blanket. When you're all warmed up, remove the heat and, with the heel of your hand, massage your own belly, picturing a clock. Find the "time" on the clock that needs special attention, keeping the massage gentle, slow and consistent. You might need 10 - 15 minutes to massage, then 5 more minutes to repeat heat. This stimulates blood flow, mobilizes your fascia and organs and distracts the pain nerves from being cranky. Yoga Yoga is a way of learning to breathe, release, strengthen, move and approach life with ease. Some of the yoga poses that relieve period pain are Child's Pose, Knees to Chest, Forward Fold, Cat-Cow, Windshield Washer Spinal Twist and Savasana. An experiment of one: Try by adding 2 yoga "classes" (at home or in a class) per week for 3 months. Employ low belly breaths, releasing your pelvic floor, heated tummy massage. Keep track of your periods for 3 months. Benefits may include: reduced cramping intensity and length of time, less moodiness, more regular periods, lighter bleeding, less bloating, less tender breasts, better sleep, improved concentration and a more relaxed experience. Find ease in your monthly cycles……they'll be a monthly experience for most of your life, so find what works for you! POP, Not the Fizzy Kind!
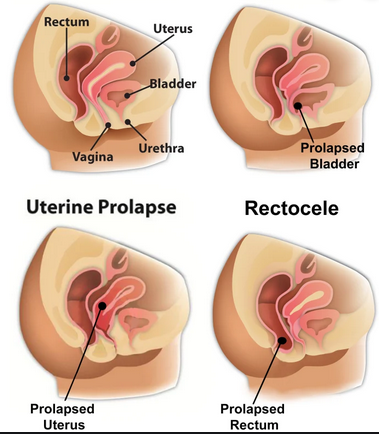
POP, Pelvic Organ Prolapse, is experienced by almost 70% of women, yet fewer than 28% of us know what it is! Let's define it, unravel its causes and Most Importantly, learn how to assess, stabilize, prevent and reverse POP. What is Pelvic Organ Prolapse? The International Uro-gynecological Association defines POP as "the bulging/herniation of one or more of the pelvic organs (uterus, vagina, bowel and bladder) into or out of the vagina." POP occurs when the muscles, ligaments and fascia (a network of supporting tissue) that hold these organs in their correct position become weakened. POP is common because its causes are so common: pregnancy, labour and childbirth, aging and menopause, genetics and family history, obesity, chronic cough, chronic constipation, heavy lifting (work or play), hypermobility (naturally stretchy people) and pelvic surgeries (especially hysterectomies). Often the impact on supportive structures earlier in life (i.e. pregnancy) that create prolapse will not be functionally obvious until menopause. That's why being assessed for POP at any time in a woman's life is so helpful…..it is usually preventable! How would you guess that you have POP? Women describe heaviness or a dragging sensation in the vagina or pelvic floor, a lump or bulge in the vagina, aching discomfort in the pelvic region, urinary or bowel problems, a dull backache or sexual problems. These symptoms often worsen with activity or simply as the day goes on. Bladder and bowel problems involve incomplete emptying, feeling the need to bear down or use manual help to finish the job on the toilet. If the bladder prolapses on its own, it can create chronic bladder infections. This is due to kinking of the bladder neck before you've completely emptied leaving just enough urine behind to brew up another infection. POP must be assessed functionally, graded, on repeated testing and with an understanding of the deep core system and breathing patterns. Our bodies are supremely clever at recruiting "help", but often those patterns of recruitment cause further dysfunction. What can you do about POP? Reversing POP is a new and exciting world in Pelvic Physiotherapy. We used to think that surgery was the only option…….a challenging surgery and one that is oft repeated due to structural failure as life's activities challenge the repaired structures. In a recent study in Vancouver, 79% of prolapse surgeries were cancelled after 8 weeks of pelvic physiotherapy, thereby avoiding the risks inherent in surgical intervention. Creston has a bounty of options for you: Pelvic physiotherapy will help you to make the changes necessary including: integrated pelvic floor and deep core muscle training, establishing healthy bladder, bowel and lifestyle habits, and learning healthy ergonomics for coughing, toileting, lifting, sport/exercise and sitting/standing/resting your body through the day. Pelvic Physiotherapy is available at Full Circle Health Centre with Joanne Gailius. An assessment and a few follow-up sessions are usually all that you'll need. Hypopressive training is available locally at Spitfire Fitness with Jenn. Group and individual Pelvic Yoga Therapy is at The Yoga Room with Barb. With your gynecologist, you may be fitted for a pessary, a ring that is inserted in the vagina to hold up the organs. After trying all conservative options, you may need surgery. You'll be ready and able to employ all the skills that you've learned already and you'll have greater benefit from the surgery! Pelvic Organ Prolapse is common but not normal. Learn about your pelvis, your deep core strength and a strong and healthy body through life's seasons. Written by Joanne Gailius, September 2018
Pelvic pain is complex and has many faces. We've talked about Painful Periods, Endometriosis and now we're going to tackle Bladder Pain Syndrome. Bladder Pain Syndrome may have begun like this: You had a urinary tract infection that just didn't go away. You felt urgency to void. You felt pain just above your pubic bones (where your bladder lives), in your perineum and/or in the urethra (the tube from the bladder to the outer world). When urinary tract infections became chronic, the old thinking was that the interstitium (bladder lining) was inflamed, ergo the outdated name "Interstitial Cystitis". Bladder Pain Syndrome is far more complex, the name far more descriptive. In 2018, we know the onset of BPS is more like this: Your bladder thinks that it's under threat…..a grizzly is at its door. Your bladder may have suffered at some point in your life, perhaps when you were a child (Chronic infections? Withholding voiding? Difficulty with bedwetting?). The part of your brain that worked with your bladder remembered this sense of distress. Later on in life (with puberty, onset of intimate relations, stressful situations, baby having, an accident or menopause), your bladder had "flashbacks" and kicked into that difficult memory. Your immune system pitched in, bringing on an immune response and inflammation. Your bladder nerve endings and the nerve pathways to the brain were woken up. Your tendons, muscles and fascia tightened up in order to protect the area. The outcome? You may develop a hypersensitive, overactive, inflamed bladder. As your bladder fills, it naturally stretches. That tight and inflamed bladder isn't so keen on stretching, sending a threat message to the brain. Your bladder naturally fills to 500-ish mls., but with BPS it can become painful at only 100 mls.. The bladder may also not welcome urine due to the inflamed lining, so you may feel a sense of urge to get rid of it…now! If you experience these feelings for more than three months, your brain begins to focus on the bladder, becoming attentive to all bladder sensations from a little urine to moderately full to urgency to pain! The natural voiding reflex and habits become distorted over time and your bladder forgets how to feel the "Oh, I'm getting full…..I'll have to go to the loo soonish, but no rush" sensation. The rising tension in the pelvic floor creates more problems. Toilet time naturally involves releasing the pelvic floor along with opening of your sphincters in a lovely dance. With a tight pelvic floor, your urine stream may become slow, interrupted, painful and incomplete. Intimacy may become painful. You may have an accompanying challenge with bowel release (not constipation….it's the letting it go part that becomes slow and/or painful). Your stress system and brain become alerted over time and this increases your perception of pain; it attaches it to your emotional state. If you haven't slept, are having a bad day or have stress, you'll feel BPS more than you would have otherwise. It's just all so connected. What can you do about it? Find a pelvic certified physio. You'll be asked about how your bladder functions, how often you void, how it feels before, during and after voiding, how your bowel works (loading, comfort, movement, frequency), pelvic floor function, deep core function and how your life is working (your nutrition, sleep, understanding of pain, pelvic systems and stress management). Your internal and external pelvis and deep core will be assessed. Research has shown us that your pelvic floor needs to be calmed down in its hypertonicity (tension), pain and function or the dysfunction and pain in your bladder won't change. You will be taught pelvic floor releases with breathing patterns, general and specific stretches and perhaps the use of a wand (a pelvic trigger point tool for you to use). An elimination diet is helpful, but no two women with BPS have the same dietary triggers. Eat food that agrees with you. Get good sleep and downtime. Find and manage your stressors. Bladder Pain Syndrome can be managed well. You can experience a cascade of wonderful changes when you take charge of your own health. |
Archives
January 2024
Categories
All
|





 RSS Feed
RSS Feed
