|
How to Fully and Completely Empty Your Bladder
or How to Void Well (pee, tinkle, wee, widdle, micturate, go to the loo……) First, what is normal, healthy voiding for an adult woman or man? Think about each of these statements and ask yourself, "Does this describe me?"
Now…..when you arrive at the toilet, there are some tricks to keep in mind.
**Not to be copied without permission; property of Full Circle Physio Creston** Joanne Gailius, BSR, PT/OT Women's Health, Pelvic and Oncology Physiotherapist Full Circle Physiotherapy C2 - 1204 NW Blvd. Creston, BC Ph 250-254-3494 Fax 1-855-655-5281 [email protected] Mar 2020
0 Comments
What is IBS?
Hint:****It's not all in your bowel, but it's the brain to bowel, bowel to brain, round and round interaction.....so think about IBS in a holistic way and read on......many of us who have "had" IBS all of our lives have no pain any longer, no bloat/distension, no suffering once applying all these principles and practices. It's SO worthwhile! And it's bespoke - sleuthing out your particular triggers and factors is a job and often takes 6 - 12 months. Hang in there and enjoy the journey! Irritable Bowel Syndrome is a collection of symptoms that add up to a diagnosis of IBS. It’s not a disease and there are no tests that can confirm or deny this name being attached to you! It’s mostly women (twice as many women as men), can be affected by hormones (worse at times of the monthly cycle and often worsens during postmenopause, when you’re one year past your last cycle). The Rome IV criterion for IBS are:
What to do? What to do? IBS is often a diagnosis given to folks when all tests of the digestive system come out “normal” and you’re still experiencing pain or discomfort, bloating and sensitivity to foods. There are medications, but long term and large studies since 2020 have shown that there are much more effective systemic (whole body) ways to address IBS. The interesting and surprising part of the studies is that medications are NOT the most effective treatment. They’re a great place to start, to help you desensitize your digestive system, but long term benefit is gained from a committed multi-pronged approach in which you discover what triggers your gut and what reduces your gut sensitivity. Everyone is different, so you are the sleuth that treats yourself best.
Property of Full Circle Physiotherapy – not to be copied without permission with thanks. Joanne Gailius, BSR, PT+OT, Physiotherapist (Pelvic, Women's Health and Oncology) C Lower - 1204 NW Blvd. Creston, BC Ph 250-254-3494 Fax 1-855-655-5281 [email protected] Strategies for Menstrual Health or Taming Your Periods
You'll have about 400 periods in your lifetime, so track them, learn about your experience and how to thrive before, during and after each cycle.
Try one idea at a time to learn what works best for you. You are unique as are your cycles. What looks like a good idea for me? Practical? Applicable? During, before or after my period begins?
Property of Full Circle Physiotherapy, updated July 2022, not to be copied without permission. JG Whatsa Prolapse and What Can I Do About It?
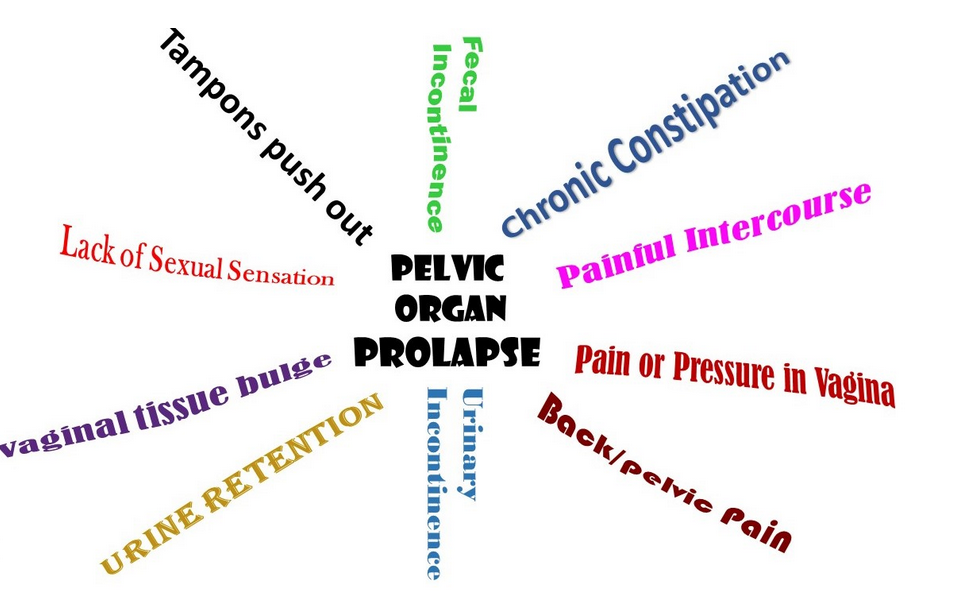
Long time, no blog. My apologies! It's time to get back in the proverbial saddle (no horses on the farm anymore) and blog a bit…… it's all in the effort to help women and their healthcare professionals, their partners, friends, sisters, coaches and more understand women's amazing bodies. So……whatsa prolapse? Most women experience a pelvic organ prolapse or dropping of their pelvic organs at some time in their lives….it's in the neighbourhood of 70% of us, depending on which study your read. Dropping or descending of your bladder/urthrea, rectum/lower bowel, cervix/uterus (and rarely your small intestine and other higher-up organs) is common; it feels like pressure, weightiness, a dragging sensation that is often relieved by lying down (overnight), antigravity positions (legs up the wall) and penetrative sex with a man (the penis helps nudge things back in place). As we work through our day and especially when we're doing a lot of heavy leaning forward and effortful work, we notice the pressure in our pelvic floor, the vagina (the inside) and the vulva (the outside) more and more. Why does this happen? Life and all its experiences and joys and challenges can bring prolapse into our lives. Think pregnancy, labour, delivery and postpartum times…..pregnant heaviness on your pelvic system, pushing hard in delivery for more than one hour, a tear or episiotomy at your perineal body (the thick and strong spot between your anus and the base of your vulva) and lots of leaning forward work of new parenthood (breastfeeding, diapering, bathing, snuggling on a tired and hormonally released body). Having multiples (yay fellow Moms of twins and more!), babies who arrive at more than 8 pounds, forceps and vacuum deliveries, more than 3 deliveries also add to the mix. Then, you might add in being overweight (belly fat adds downward pressure), having a persistent cough (asthma, COPD, smoking, allergies….), doing heavy physical work, doing leaning forward work (sitting, gardening, lifting +++…), chronic constipation/bearing down on the toilet and impact sports (basketball, running, power lifting….). How we sit (cross your legs/feet and slouch), how we breathe, how we move, how we live in and above our pelvic system adds some more prolapse factors. Now……think about lovely postmenopause. Remember that menopause is that moment when you are one year past your last cycle. You shift from perimenopause to postmenopause in an instant. The loss of spunky estrogen, the hormone that supports your muscles to be active, thick, juicy and responsive, means you lose some of the natural hormonal support of your organs. After reading this list, you see why most women prolapse at some time in our life. How do we test for prolapse? We pelvic physios follow a testing protocol that is well researched and supported. During your pelvic exam, we figure out where your organs are at rest, then we ask you to take in a deep breath and bear down. We measure, with our finger or a POP stick, the descent of the organs down your vaginal vault. The "gold standard" of testing involves you doing 6 repetitions of 6 seconds of bearing down with a wee break in between. But, that's not all! We also measure the quality and speed along with the amount of natural retraction of your organs between each bearing down. We might ask you to lift your pelvic floor, to try a different position, to breathe out with an anal squeeze or a hypopressive manoeuver so we can sleuth out how you can help lift your organs yourself. It's all about finding out what works specifically for you once we see that you're prolapsed. We "stage" the prolapses out of 4. If you have a stage 1 prolapse, it's pretty minimal and possibly inconsequential……this means that your organs are descending to less than ½ way down your vaginal vault on bearing down, it doesn't worsen as you repeat it and they mostly return to their starting position in between. If you're at a stage 2, your organs are descending to the "introitus" or the opening of the vaginal vault at the vulva. At stage 3, the organs go beyond that and poke out past the opening and stage 4 means they're mostly living there. Women at stage 3 and 4 might describe a constant pressure that worsens with toileting and a scraping or bulging on wiping after BMs and voids. Why do prolapses happen? Big friendly letters - It's Not Because You Have a Weak Pelvic Floor! Repeat after me!!!! Prolapses happen because your pelvic organ support system, the core cylinder of your central body, has some pressure management fault. There is a natural support system on every breath and every movement that moves your thorax to abdomen to pelvis that involves your pelvic organ support. It's supposed to keep supporting your organs as you go through life! But there are times in a woman's life when we ask more of the system than the support system can manage, so we develop coping strategies that create prolapse and/or we don't find pelvic organ lifting as we need in a day. What can you do about it? Brace yourself - SO MUCH! Simply change how you breathe, sit, move, eat and toilet and you're all set! If you have an intractable stage 3 or full stage 4 prolapse, you'll be referred to a gynie surgeon who might offer to tack up your organs onto your pelvic ligaments/fascia. But, please see a pelvic physio in the meantime so that the habits and situations that caused your prolapse are sleuthed out and you don't return to said surgeon for round #2. At stage 1, you're probably post partum or early perimenopause and might be just fine. I'd still recommend that you check it out with a pelvic physio so that your prolapse doesn't progress. Stage 2 and early stage 3 brings you the opportunity to meet in the clinic - you can learn to lift your organs with some lifestyle changes, some adaptations to what and how you do what you do, some strengthening and postural exercises and perhaps referral to other options like hypopressive training, postural work, yoga therapy and more! Don't stop doing what you love to do but learn to do it with joy and employ clever lifting of your organs. As a previously prolapsed postmenopausal woman, I run, work hard on our farm, lift haybales (repeatedly and often) and am no longer prolapsed. It takes attention, training and time, but it's so worthwhile. What else do you need to know? You may have postmenopausal urogenital syndrome (vaginal atrophy) that's contributing to your prolapse. Address that. You might have interrupted or double voiding or persistent urinary tract infections. Address that. You might need to splint your anorectal system to poop effectively or be constipated all the time. Address that. You might have other spinal issues that are contributing. Address that. If you're carrying extra weight on your tummy, it's pushing on your prolapse. Address that. And your cough, COPD, smoking, allergies, posture, heavy lifting……what things can you begin to address that will already help your organs lift and be perky again? The important bit = Prolapses happen to most of us and are common, but they're not normal nor acceptable. Ask at your next PAP smear or seek a pelvic physio to help you learn to have happily supported pelvic organs, a strong deep core, brilliant voiding and pooping and a happy pelvic life throughout your seasons! Bloating Bellies
Many people suffer from bloat - that inflated, super sensitive belly that happens when you eat something that doesn't agree with you, you get stressed, you go out for dinner (and eat something new + are socially stressed), you _______......there is usually a story that you recognize. And it's both possible and plausible to prevent a painful, gassy bloated belly as well as manage it yourself with a few nudges, learnings and cues. Let's sleuth out bloating bellies. Bloat is that pesky experience when your belly feels tight, puffy, gassy and can be somewhere between uncomfortable and really painful! As with many conditions that pelvic physios address, this may or may not be a medical (see your doctor) issue. Bloating may be more of a functional issue, a challenge that interferes with you enjoying life's adventures or traveling, a colourful and yummy variety of food (Cue #1: Remember to go for 30 different plants per week…..grains, seeds, nuts, vegies, fruits, legumes), dinners at restaurants or friends' homes and socializing in general. That makes bloat a human issue! What causes bloating? One common cause of bloating is constipation (Cue #2). You can be constipated and not realize it, since having fewer bowel movements, smaller BMs or BMs less often than you normally do are just a few symptoms of constipation. You may still be constipated even if you have regular bowel movements. The longer your stool stays in your colon, the more time the bacteria have to ferment what's there, resulting in more gas and bloating. We think about constipation in a variety of ways, including how you have a BM (positioning, starting, stopping, texture, stickiness, effort needed etc.) and how it might change under different circumstances. Remember that your bowel thrives on boring, consistent, regular……and it deplores change of any kind!
What can we do about APD?
What is PF? Proctalgia means pain around the back passage area (anus/rectum) and/or, for some women, into the vagina. It's most often a central spasm + pain and less often appears on one side more than the other. Fugax is a Latin word meaning fugitive or fleeting, so it's a pain in your anus/vagina that's like a spasm and is short lived……a squeeze and gone or a deeply unpleasant clench that can hold on for a 2 - 20 minutes. Pain can appear frequently over a few weeks, each time lasting only seconds or minutes or appear rarely and only during specific actions/activities. It is a sudden, cramping, severe pain that may make you feel nauseous and quite awful. It may wake you up in the night. If the spasm builds and becomes difficult to release (feeling "locked in"), you may have aching for up to a day afterward leaving you with a tired + tender anus/vagina that makes lengthy sitting uncomfortable and release for toileting and intimacy unpleasant. About 1 in 5 people have PF, so this is worth attending to! A specialist once told me "you just have to live with it". If you've been told that, read on. This isn't because doctors don't know about PF, but reflects that they can't test it or see/palpate it, because you're not usually in their office when it clamps on. Then it passes, so it's not really a huge or impactful medical issue, but it IS a functional issue that has had very little attention…..until now. Your doctor can rule out other problems that may cause similar symptoms, so please mention these anal/vaginal spasms to them! Then find a pelvic physio to assess your pelvic floor. You can begin by reading onward and seeing if this story and these suggestions help you to reduce the frequency and intensity of your PF, then help you bid PF goodbye! It is treatable, manageable and you can stop it from coming on. This requires attention - when you have PF, take stock of your life, activities, rest, stress, food etc. at the time. Ask yourself what was going on just before or within the last ½ day? Jot it down on the calendar or in your in notes on your phone. Next time you experience PF, write it down again. Pay attention to your triggers. Shared problems may include: IBS or an IBD? Bloat? Abdomino-phrenic Dyssynergia? Overactive pelvic floor? Urge/urge incontinence for your bladder? Overactive bladder (pee too often)? Pain with sex? Sluggish/painful bowel release)? Hemorrhoids? This pesky list reflects pelvic diagnoses that also occur with an overactive, hypertonic or hyperrecruited pelvic muscle system. Find your Triggers. There are numerous triggers for PF including sexual activity, stress (+++) of all varieties and blends, grief, constipation, bowel movements, during/right before periods, sport activity like speed walking/running/interval work/hill work, gymnastics, basketball, sudden start/stop sports like softball or baseball …….although the PF can occur without a trigger. Increased stress (physical, emotional, relationship or a blend thereof) is most commonly implicated due to our very human tendency to protect ourselves by "holding on" when stressed. We do this by butt gripping, pelvic floor clenching and tensing our lower abdominals (especially the Transversus Abdominus muscle just above your pubic bones). Some of these muscles share attachments with your anus (external anal sphincter) and your vaginal walls (too many amazing muscles to list) and they all share the same electrical circuits (neuromotor or nerve to muscle communication). Nerves (and muscles) that wire together, fire together. Notice onset (like an aura with a migraine). Some people describe a sensation of lifting or tightening of their pelvic floor or a very mild ache in their deep buttock or anus prior to the onset of PF…..notice it and begin emergency measures immediately. You can learn to stop PF from coming on to a full clamp. Immediately apply emergency management measures! You need to release a spasm, so think of PF like a foot or calf cramp….it takes work + calm + time + skill. Begin by taking deep, pelvic-diaphragmatic breaths, inhaling fully for a slow count of 4, then releasing it with big (Dizzy Gillespie playing the trumpet) cheeks or a deep bear growl or a long, slow, groany groan. If you're near a toilet, sitting on the toilet seat (not the lid) with your feet planted on the floor and your elbows on you knees ("reading the newspaper on the floor position") can be helpful for 2 reasons: you're used to releasing your pelvic floor on the toilet (habit) and the toilet seat is built to open up your pelvis (that sinking down in the middle). It's a good tool! Imagining release (motor imaging) of your pelvis, anus, vagina, buttocks, low belly and hips helps, so picture it while releasing with your mind. Go to your Savasana or meditation or beach or post-run feeling in your mind. Positions that might help: squat (on your own or with your sacrum on the wall for support or at the wall or with a yoga block or low stool under your buttocks), hinging at the hips with your palms or elbows on your thighs, wide kneed child's pose or happy baby. In all these positions, release your anus and vagina, especially on a deep and low in-breath with back pressure outbreath (big cheeks or bear or deep groan) so that you find ways that you (when you're not in spasm or pain) can release, release, release. Do some prevention movement, breath practices and stress management daily. Ask your pelvic physio to help you learn to turn OFF your pelvic floor and lower abdominals; we call this downtraining or quieting. Do this practice every day for 2 weeks, then continue on most days, reminding your lower muscles, the centre of your deep core, that activation is OK but release is brilliant too! Learn to do pelvic diaphragmatic, 4 part, back pressured out breath (big cheeks, bear or groan) or Dirga breaths as part of your "release your body and mind" practices each day. You don't always breathe this way but it helps you to know when to use this technique for the right moment (toileting, sex, birthing, PF). Never grip your buttocks nor hold your tummy in - these are really unhelpful habits. You're beautiful as you are and gripping/holding doesn't help. Learn where "your body keeps the score" - find those spots in your own body where you "hold on" and notice when you're feeling the urge to protect, get stressed out or overwhelmed and learn to release them. Responding fully with a calm body to stress without being stressed out is a wonderful thing. Make squatting and/or happy baby and/or child's pose or leaning forward with your hands/elbows on your thighs a stretch that you include in your day, especially before/after situations that often trigger you. And breathe deeply and fully into the stretch, feeling the release and enjoying the moment. Joanne Gailius, BSR, PT+OT, Physiotherapist (Pelvic, Women's Health and Oncology) C Lower - 1204 NW Blvd. Creston, BC Ph 250-254-3494 Fax 1-855-655-5281 [email protected]  Toileting Tricks Position Sitting with your feet solidly supported on a stool/yoga blocks, knees slightly higher than your hips, completely calm and relaxed, leaning forward slightly ("reading the newspaper on the floor") position is often helpful, but not always. You're looking for release of your pelvic floor (especially your puborectalis muscle) and a straight anorectal angle so that the rectum is a direct highway. You can try this by going to the bathroom when your bowel isn't cueing you for a BM, closing the toilet lid, sitting down on it, feeling your tailbone and/or anus and trying which position, breath pattern, knee height releases your very own system. Pressure Management This happens at your glottis (throat/larynx) and involves you finding which noise/action opens your glottis to that Goldilocks perfection of releasing your pelvic floor and anus. Try these by sitting on your toilet lid (as above) and noticing….When does my anus open for a free and calm release? Look at the photos above for cues....... Grrrrr………………..Shhh…………….Mooooo……….Sssss…………….Straw blow………….Dizzy Gillespie cheeks…… Sometimes You Need External Support (with rectal prolapse and/or deer pellet poops) With your finger just ahead of your anus on the Perineal Body, inside and onto the back wall of the vagina or using a Femmeze to push that "R" pocket back towards your buttocks and make the passageway straight. Best Stool Shape, Consistency + Size You're seeking a smooth, long, snake-like, Bristol Stool Score #4 stool…..what eating + drinking + fibre + stress management + movement + sleep support do you find that works consistently for you to create that? Find it and repeat. Try for a BM 20 - 30 mins After Arising/Drinking, Before Leaving Home Try to teach your colon and whole system that a morning, post-arising (moving), post warm drink, pre leaving the house BM sets you up for a good day. Effortless, releasing, calming, restoring, empty-bowel-for-the-day kind of routine. Breath Patterns that Help You Play around, feeling your tailbone/anus…..what breath actions help you release. Is it low, slow, deep, pelvic breaths? Big cheek puffy breaths in and out? Saggy body, open hip breaths? Find your best breath pattern and repeat, repeat. Make Toilet Time a Priority No tech, no cellphone, no ipad, no lists…..don't take toileting for granted. Make time (get up a little earlier) to toilet well, fully and completely, without effort and with calm, soft release. See if you can be in the bathroom alone and teach your family that this is you-time…..that you're a happier and healthier you if you have solo toilet time. Pooping Away from Home may need sound support (turn on the fan) + Confidence of Privacy (lock the door) + Reducing Odours (make + use the Poop Spray) If you don't have a BM prior to leaving home in the morning and it just doesn't become your habit despite attempting to teach your digestive system to do so, you may need to have your bowel release during your outside/work day. Use all the best tricks (sound, privacy, poop spray) to make it happen regularly, confidently, calmly and with consistency. Poop Spray Essential oils (orange, grapefruit, lavender, peppermint), 15 drops 2 T. vodka 1 drop dish soap water to fill bottle Pre-pooping, shake the bottle well and put 4 squirts into the bowl prior. The spray will catch the odours and it will all flush away. Joanne Gailius, BSR, PT+OT, Physiotherapist Jan 2023 (Pelvic, Women's Health and Oncology) C Lower - 1204 NW Blvd. Creston, BC Ph 250-254-3494 Fa Hello friends of Full Circle.
It's a time of year when stress may nip our heels. Have a read through this list....ponder on what you can begin, with a sense of playfulness, even delight.....what would be fun to try, to repeat for a week or two and see how you feel. Calmer? A little more ease? Less frantic? Tummy less cranky? Reduced pelvic pain? You are the expert about yourself and your own body. What would make today more colourful, more vibrant for you? Daily Gratitude List Write down 3 things for which you're grateful today. Keep going if you'd like to, but create a habit of finding 3 things or people or daily activity or interaction or weather or ______ that you noticed gratitude about. Move Your Body Go for a 10 minute walk or jog or toodle down a quiet road or through the forest…..no phone, on your own, no distractions, noticing the temperature, the humidity, the clouds, the trees. Just be present in the moment of moving in the world. Go every day, growing your movement to 30 minutes each day. Even the stormy, snowy, windy or rainy days can be brilliant! Breathing Ideas Pick one of these breathing ideas and do any of these 10x in a row, notice if you feel calmer. Then repeat daily (or whenever you feel your shoulders rising, jaw tightening or butt/toe gripping). Or try another and play! So Hum As you breathe in say (or think) "Sooooooo…." Then as you breathe out slowly, say (or think) "Hummmmmm." Alternate Nostril Breathing Place your fingertips #2 and 3 on your forehead. Use your thumb tip to close your R nostril. Breathe in your L nostril. When you're full of air, use fingertip #4 to close off your L nostril and breathe out your R nostril. Don't move your fingers when you're empty of air. Breathe in your R nostril. Full of air = switch fingertips on nostril closure so you breathe out your L nostril. Breathe in your L nostril and repeat. Slowly. Deep Pelvic Breath Ly or sit in a comfy chair. Place one palm on your chest bone and one on your low belly, releasing your belly, buttocks, hips and pelvic floor. Breathe in your nose, slow and deep with only your lower hand lifting with your filling belly, feeling your hips release, your pelvic floor (vagina/scrotum/anus) open and widen and your back arch gently. Breathe out your pursed lips, slowly and simply letting your body release and let go….no action, just settling back to the starting position. Distance from External Expectations Reduce the power and proximity of societal, familial, friend (other) expectations in your mind, body and self-talk. Step back from Facebook, Twitter, Instagram, You Tube, your cellphone. Take at least one day unconnected to it all. Notice what matters to you (not others). Greet the Woman in the Mirror As you wash your face and brush your teeth in the morning, greet the woman in the mirror and thank her for coming into the day, taking care of herself, being her/you. Notice how you look, take time to appreciate your eyes, your smile, your presence. All that you bring into the day is improved if you're thankful to be you. Sleep Well Invest some commitment, time and energy into sleeping well. Stop all scrolling/watching/phoning 2 hours prior to a consistent, calm, warm bedtime. Make bed time routine and sleep a really important part of your daily commitment to a healthier, calmer, more vibrant you. Connection Where, when, how and with whom do you fill your cup? Is there a weekly visit with someone that you'd find energy-giving? A weekly walk with someone, a teatime, volunteering, checking in with _______? Creativity Everyone is an artist and has a creative urge that support each of us being ourself……Cooking? Baking? Drawing? Knitting? Painting? Journaling? Photography? Hands on, expressing you being you. Unitask Once your estrogen is depleting/depleted (peri to post menopause), your cortisol (stress hormone) will rise if you continue to multitask. Estrogen helped you multitask; you don't have it any more. You'll ask your stress system to respond if you keep multitasking, so stop it! One task, one activity, one skill, one thing at a time. Prioritize and do one thing. Then stop and appreciate that you've done "it" and go onto the next one. Way less stress. Compassion Self Compassion (Self-compassion entails being warm and understanding toward ourselves when we suffer, fail, or feel inadequate, rather than ignoring our pain or flagellating ourselves with self-criticism) and Fierce Self Compassion (Fierce self-compassion involves “acting in the world” to alleviate suffering. It tends to involve protecting, providing for, and motivating ourselves. Sometimes we need to stand tall and say no, draw boundaries, or fight injustice. Or we may need to say yes to ourselves, to do what’s needed to be happy rather than subordinating our needs to those of others. And if we’re stuck in a bad situation or habits that are harmful, it means doing something different. Not because we’re unacceptable as we are, but because we care.) Definitions by Kristen Neff with gratitude for her two books. Noticing All of us have stress in our lives. In fact, we need a modicum of stress in order to be alive! In addition, some of our stressors aren't changeable ….. our family, our health concerns, our aging parents, our jobs, our financial position. But…..we can notice our "body keeping the score". Are you A jaw clencher? A shoulder holder? A butt gripper? A toe grabber? If your body continues to "keep the score" of all of life's stresses/stressors, do you respond further by Not sleeping? Developing a headache? Catching the latest virus passing by? You can change up your stress response by first noticing how you in your "only you" way respond to stress. AHA! Paying attention is surprising and enlightening. Then release your jaw, soften your shoulders,you’re your tummy go, rock back and forth on your toes while you release your buttocks and wiggle your feet. Just breathe. Repeat with your inbreath, "I am safe", and with our outbreath, "It's OK to let go". These small ideas can change your sense of calm, your response to life's challenges and your vibrancy. What works for you? 1. _______________________________________________________________ Date: ___________________ 2. _______________________________________________________________ Date: ___________________ 3. _______________________________________________________________ Date: ___________________ C2 - 1204 NW Blvd. Creston, BC Ph 250-254-3494 Fax 1-855-655-5281 Fertility Facts Fertility Difficulties are complex and are important to sleuth out with the help of specialists (OBGYNs, both general and specialized), Urogynecologists (particularly for those with persistent pelvic pain), Other specialists (eg. if you have UC or CD, your Gastroenterologist or if you have RA or Lupus, your Rheumatologist) and your GP/NP. Fertility challenges are 40% due to the female partner + 40% due to the male partner + 20% of unknown/interactive (i.e. woman's allergic response to the man's sperm) issues. 1 in 6 couples in the UK sought fertility help in 2019. Over 80% of UK couples will conceive within 1 year of trying and a further 50% of the remaining will conceive within the second year. When we struggle with fertility, it's an often overlooked, challenging, difficult journey (ref: youtube channel of Lauren Mancell (https://celebratemuliebrity.com/2018/09/trauma-awareness-in-womens-health/). 30% of all pregnancies end up in miscarriage. A Woman's "Normal" Cycle
- luteal stage = holding, implanting, high progesterone (maintaining implantation) Know When You Ovulate and Track it Yourself Duration of cycle Ovulation day 22 day cycle day 6 - 10 24 day cycle day 8 - 12 26 day cycle day 10 - 14 28 day cycle day 12 - 16 36 day cycle day 20 - 24 32 day cycle day 26 - 30 Ovulation Information Mittelschmertz - a stabby kind of pain on one side of your lower pelvis when the egg is released. Your mucous is like egg white (stretchy, springy) and is more receptive to sperm, drying out a little after ovulation passes; the neck of your cervix is more open and welcoming. Your basal body temperature (taken first thing in the morning, prior to arising/warm drink) dips slightly at ovulation and rises slightly in the luteal stage. Keep a pen, paper (or phone tracker) and thermometer right beside your bed. Test and record your temperature daily and learn about how your body navigates the monthly-ish cycle. This is to create self-knowledge and to provide helpful information, not for complete focus. It's a "know thyself" moment. A BMI of >19 and <30 is the "golden window" for conception. Habits that help: no alcohol, no smoking, active lifestyle, manage diseases (Hep B/C/HIV), avoid occupational (chemical) exposures, wear loose-ish undies (especially the men), manage/address Endometriosis/PCOS/PID before/during fertility times, wait 3 - 13 mos. after coming off OCPs (the pill) while your body re-establishes its own natural hormonal cycles, avoid use of Ibuprofen (Advil, Motrin). Specific Dietary Recommendations: Mediterranean Diet, plant focused (at least 5 plants/day with a variety of up to 30 different plants per week), nutrient dense, organic/healthy protein sources that aren't processed, add Omega 3's that are algae based, look at your micronutrients (Folic Acid, B12, Zinc, Iodine, Vit D, Selenium, Iron with Vitamin C and without caffiene), Dairy should be high fat, Eliminate transfats, meat < 3x/week with fish > 1x/week, pass on alcohol + caffiene for both women and men, All the Dietary Recommendations equally affect both partners! Sleeping well/restoratively/consistently + Stress management/reduction are hugely important in themselves and need their own special focus! Daily exercise - some cardio, some strength, some flexibility, some restorative….."moderate physical activity" boosts conception success (including IVF) so think Goldilocks (not too little, not too much, just right). Get your hormonal profile checked if you're over 35 or not successfully pregnant within 1 year of trying and/or if you've had miscarriages (2+) to track/check your ovulation and/or have had 3 miscarriages. Egg Meets Sperm Facts Your egg is ready/fertile at 24 - 28 hours after you ovulate. Your sperm can be lively/ready to fertilize an egg for 5 days after being released in a hospitable environment. Find a Pelvic Physio trained in Fertility Support Manual Physiotherapy doubles IVF success rate (specifically myofascial + lymphatic + visceral) by improving the mobility/health of the implantation neighbourhood. Ongoing studies suggest the same result of these therapies for natural pregnancies. Addressing depression + anxiety is helpful. Studies recommend calming yoga (gentle hatha, restorative and/or yin) + Cognitive Behaviour Therapy + mindfulness practices + lifestyle changes to improve sense of self-efficacy and confidence. Consistency is the key, trying one new practice at a time for 4 - 6 weeks, 4 - 7 days/week before adding a second change. Remember small, consistent baby steps (1% change per week) is the best and most helpful, long-term approach. Weight management is vital for both partners so that BMI is stable between 19 and 30. Managing and stabilizing all chronic diseases including coeliac, endometriosis, adenomyosis and PCOS particularly. Cease smoking asap for both partners (refer to Alan Carr's "Easy Way to Stop Smoking" book). Addressing sleep disorders is vitally important as sleep is restorative and a key health factor. This means consistency with bed times, awakening times, cool room, warm feet, darkened windows, quiet or white noise, no blue light 1 - 2 hours prior to bedtime, no cell phone/ipad/laptop in the bedroom, warm bath/shower prior to bed, no snacks after 7 pm….make restorative sleep a priority. Identify and address all physical + emotional + relational stressors in your life. Craft a life that is calm, enjoyable, consistent and with comfort, predictability and joy. If you've had a miscarriage (or 2,3), you may feel loss and grief. It may help to speak with someone with whom you can be vulnerable and open. If you're able to be open and find support, it may help lift the veil of grief for you. IVF adds a whole new adventure/challenge. You may experience heightened anxiety when patience and care, sensitivity and support are what you need. Practicing daily/consistent mindfulness, breathing practices, progressive muscle relaxation and pelvic relaxation/release may be helpful. You may find that psychotherapy (particularly CBT) is an additional self care strategy. Biofeedback (self-taught or mindful training) to reduce stress hormones + improve sleep are recommended. Big self care, self compassion and calm are the bywords to repeat. Your individualized plan:
Property of Joanne Gailius, Full Circle Physiotherapy, Not to be copied without permission.  Inflammatory Bowel Disease (Ulcerative Colitis (UC) and Crohn's Disease (CD)) What does a pelvic physio have to offer someone who has IBD? Top Down (stress management + sleep challenges + microbiome support + exercise prescription + lifestyle factors + individualized concerns re: work/play/restoration/meaningful activities) Bottom Up (anal incontinence and/or constipation + bowel functional support/education) treatment, bladder + sexual + pelvic organ support + systemic challenges (skin, joint, eyes…) Focus: What's happening now? What is getting in the way of you enjoying your best, most meaningful life? Write your very unique list. All recent research says that lifestyle (more than medication or surgery) is the #1 most effective way to treat UC and CD or the combo. Facts About IBDs from 2015 - present research: Genetics?: Presence of IBDs has a genetic link, but there is no genetic link to the severity of the disease. Severity of both diseases is clearly linked to lifestyle/diet/smoking/stress management. These are modifiable factors and put you in the driver's seat. Stop smoking immediately (including second hand smoke) - Refer to Alan Carr's book on smoking cessation. Smoking is pro-inflammatory and your job is to reduce inflammation or "put out the fire". Reduce or stop alcohol consumption - 1 - 3x weekly of one beer, one x 5 oz. glass wine or 1 oz. alcohol. No stacking (never more than one at a time). Alcohol impedes a healthy gut microbiome and is pro- inflammatory as well! The Story of IBDs and Fibre? There is no evidence to support a low fibre diet for someone with IBD (most of the time). Fibre is protective for those with IBDs with a minimum of 27 gm fibre/day and preferably 35 - 50 gm fibre/day. It's very old, outdated advice to eat a low fibre diet. Why? - Fibre feeds your microbiome, helps control blood sugar, stabilizes body weight, helps immune regulation in your gut's T Regulator cells, maintains healthy gut barrier to reduce leaky gut, increases the mucous production to keep pathogenic bacteria off gut wall, helps excretion of excess hormones and supports your gut-brain axis (you think more clearly!). Proviso** - If you have a stricture or scar tissue limitations, you may need to eat low fibre until that is released surgically and/or with pelvic physio. Full Circle Physiotherapy and IBDs Page 2 How do you increase your fibre intake? - Low and slow is the motto. Choose one thing from the list below, see how your body responds over 2 - 3 weeks, then try the next. Keep what serves you.
Fatigue - Fatigue is a functional concern for most people with IBDs, but especially women + younger + early stage + if you have pre-existing depression and/or anxiety. Research shows that the experience of IBD related fatigue is very similar to the fatigue people experience while having chemotherapy. Why? - IBD creates an inflammatory state in your body which is anxiety provoking, your gut-brain axis is wobbly (need microbiome support…..see all dietary suggestions above), treatments/surgery are taxing, depression/anxiety/loose stool may interrupt sleep. What can I do about it? - Calm your system/put out the IBD fire, develop a brilliant and varied microbiome, help your system to reduce medical/pharmaceutical/surgical needs by caring for yourself with healthy choices and consistency, then…Practice unwavering, consistent sleep hygiene (daily consistent bedtime and awaken times, safe/comfortable housing, cool room/warm feet, quiet/calm evening routine, no blue lights 1 - 2 hours prior to bedtime, covered windows, no evening snacks, cellphone not in bedroom (no texts/emails/calls during dedicated sleep time), write list for tomorrow on paper/phone and leave it in kitchen)….find what works for you and stick to it every single day/night! Personalized Exercise Programme Daily to 3x/week aerobic + resistance (weights or body resistance) boosts your immune system's response (but studies show that it didn't change bowel function). Aerobic exercise for 30 mins. x 5/week helps support your heart health, gives you a sense of calm (endorphin release) but can activate the bowel. Keep timing and fatigue in mind. Most folks with IBD choose early morning for their run/bike/swim. Calming exercise, like yin yoga and/or a regular gentle stretching routine can help reduce stress, anxiety and promote sleep. No surprise that this can be a lovely part of an evening time to promote sleep and calm the mind. Full Circle Physiotherapy and IBDs Page 3 Mental Health Considerations
Pelvic physios are trained in incontinence of bowel and/or bladder, bowel management (constipation et al.), sexual function/dysfunction, pelvic organ support, persistent pelvic pain and more. Any of these challenges may be within the experience of those who have IBDs. Prehab and rehabilitation from abdominal/pelvic surgeries, including ostomy surgeries, is part of our work as well (scar tissue release, tendomyofascial release, posture, abdominal/pelvic recruitment + strengthening + function and more). As a very specific example, the puborectalis muscle (a sling shaped muscle that wraps around and supports the anorectal canal) can become over-recruited and tight in some people with frequency/loose stool and functionally impedes the movement of the stool as it exits. It then looks like constipation, but is actually the opposite! A pelvic physio can help with manual therapy (releasing the muscle) and teaching you to accomplish this yourself with breath, positioning, your own hands/therawand…..even how/when you toilet. Assessment and treatment are yours to choose/guide. If you contact a pelvic physio, ask if they are trained in anorectal dysfunction prior to your appointment. And if you have any questions or concerns, please feel free to email me at [email protected] and/or peruse my website: fullcirclephysiotherapy.ca. Property of Full Circle Physiotherapy |
Archives
January 2024
Categories
All
|






 RSS Feed
RSS Feed
